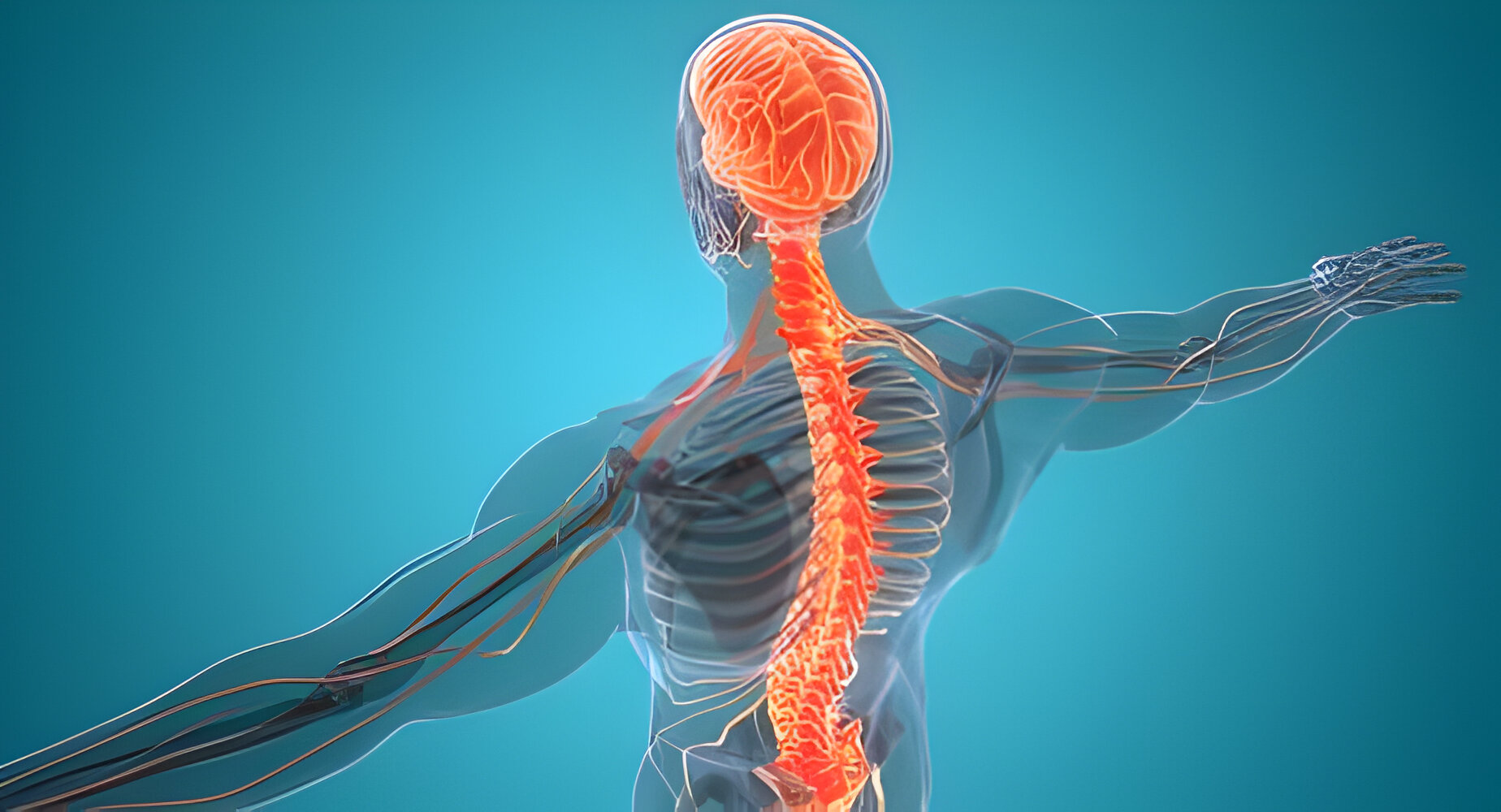
Recent scientific discoveries have unveiled a surprising link between brain inflammation and muscle fatigue, potentially revolutionizing our understanding of various diseases and their associated symptoms.
Researchers at Washington University School of Medicine in St. Louis have identified a protein pathway that connects brain inflammation to reduced muscle function, offering new hope for treating conditions ranging from bacterial infections to Alzheimer’s disease and long COVID.
Unraveling the Brain-Muscle Connection
Scientists have long observed that patients with brain inflammation often experience muscle problems seemingly unrelated to their central nervous system. This puzzling connection has now been illuminated by a groundbreaking study published in Science Immunology.
Dr. Aaron Johnson, the study’s senior author and associate professor of developmental biology, explains, “We are interested in understanding the very deep muscle fatigue that is associated with some common illnesses. Our study suggests that when we get sick, messenger proteins from the brain travel through the bloodstream and reduce energy levels in skeletal muscle.”
The research team modeled three diseases – E. coli bacterial infection, SARS-CoV-2 viral infection, and Alzheimer’s – to investigate how brain inflammation affects muscle function. They discovered that inflammatory proteins characteristic of these diseases trigger a cascade of events in the brain, ultimately leading to the production of interleukin-6 (IL-6), a molecule that circulates throughout the body via the bloodstream.
From Brain Inflammation to Muscle Weakness
The study revealed that IL-6 in mice – and its corresponding protein in fruit flies – significantly impairs energy production in muscle cells’ mitochondria, the powerhouses of cellular function. This impairment manifests as reduced motor function and decreased physical performance.
“Flies and mice that had COVID-associated proteins in the brain showed reduced motor function,” Johnson noted. “The flies didn’t climb as well as they should have, and the mice didn’t run as well or as much as control mice. We saw similar effects on muscle function when the brain was exposed to bacterial-associated proteins and the Alzheimer’s protein amyloid beta.”
Importantly, the researchers found that these effects can persist even after the initial infection has cleared. Dr. Johnson emphasized, “We also see evidence that this effect can become chronic. Even if an infection is cleared quickly, the reduced muscle performance remains many days longer in our experiments.”
Promising Pathways for Future Treatments
The discovery of this brain-to-muscle signaling pathway opens up exciting possibilities for treating muscle fatigue associated with various diseases. The researchers identified that IL-6 activates the JAK-STAT pathway in muscle cells, leading to reduced mitochondrial energy production.
Dr. Johnson highlighted the potential clinical implications: “Several therapeutics already approved by the Food and Drug Administration for other diseases can block this pathway. JAK inhibitors as well as several monoclonal antibodies against IL-6 are approved to treat various types of arthritis and manage other inflammatory conditions.”
While the evolutionary purpose of this seemingly detrimental process remains unclear, Dr. Johnson speculates, “If we want to speculate about possible reasons this process has stayed with us over the course of human evolution, despite the damage it does, it could be a way for the brain to reallocate resources to itself as it fights off disease.”
As research continues, these findings could lead to new treatments for the debilitating muscle fatigue experienced by many patients with inflammatory conditions. Dr. Johnson concludes, “We hope our study encourages more clinical research into this pathway and whether existing treatments that block various parts of it can help the many patients who experience this type of debilitating muscle fatigue.”
Sources:
Science Immunology: “Infection and chronic disease activate a systemic brain-muscle signaling axis.”